Patient’s Section
This space is dedicated to you with the aim of explaining what an orthopaedic implant is and the reasons why surgery may be necessary.
Here you will also find simple explanations about the joints for which our products are designed, allowing you to approach the operation with greater understanding and peace of mind.
The information published on this site is precisely that – information – and is not a substitute for an appointment with a practitioner.
A total hip replacement is a device that replaces the hip joint when that joint has been damaged.
What is the hip joint ?
The hip is a joint that attaches the thigh to the pelvis. It consists of the femur, the head of which bolts into the pelvic cavity. The surfaces of the joint are covered in cartilage, which allows them to slide smoothly over each other.
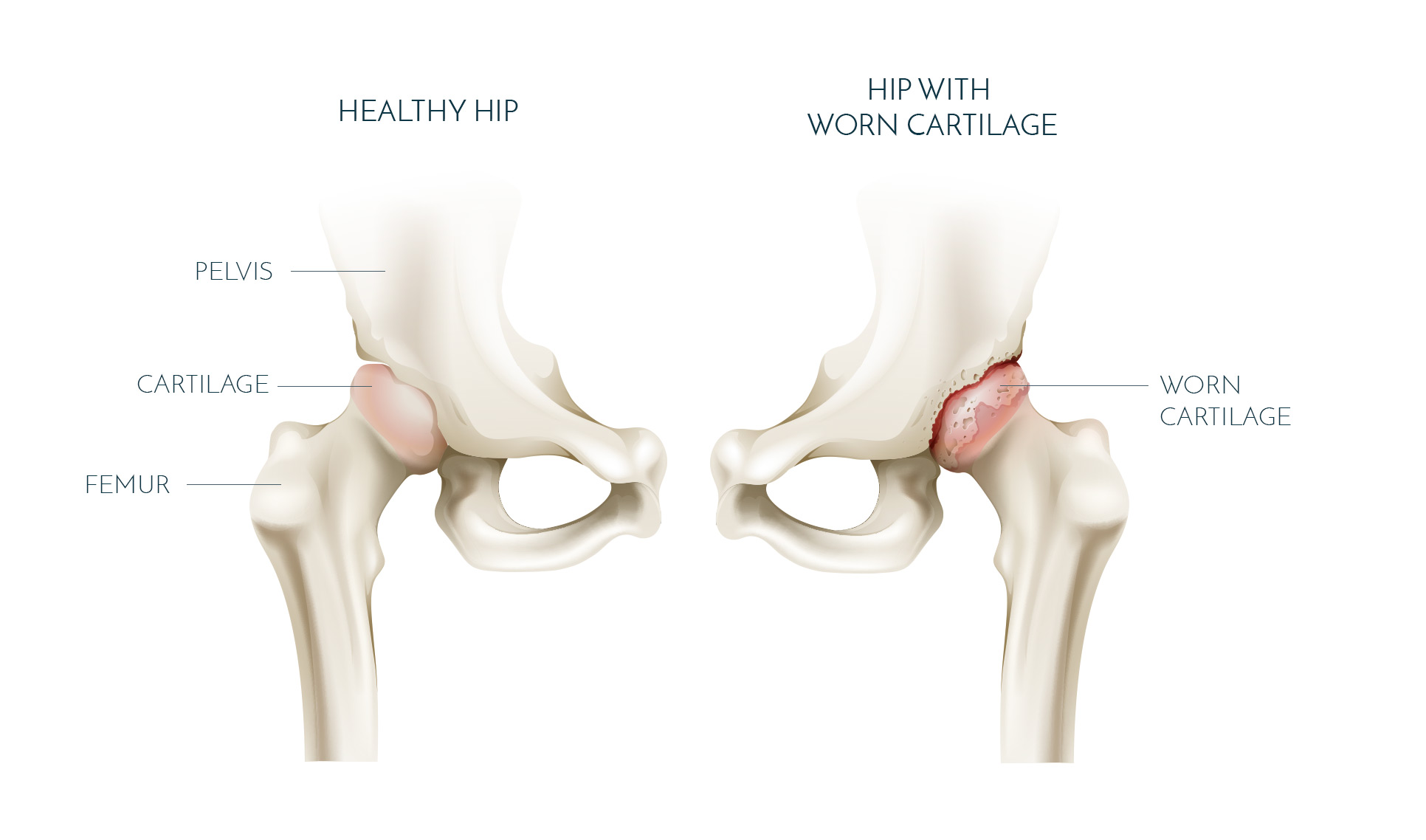
In what situations could a hip replacement be necessary?
The surgeon will carry out a total hip replacement for patients whose hip joint is worn and as such is causing pain and reduced mobility. The hip replacement is therefore a solution that reconstructs the joint, relieve pain and restores joint mobility when medical treatment is no longer sufficient.
Possible causes of joint cartilage deterioration:
- Coxarthrosis or arthritis in the hip joint
- Fracture of the neck of the femur
- Osteonecrosis in the head of the femur
- Rheumatoid arthritis
The artificial joint
- The stem, which is inserted into the femur;
- The head (ceramic or metallic) which is placed on the stem;
- The liner (ceramic or polyethylene) which allows the head to slide within the cupule;
- The cup, which sinks into the pelvic cavity.

The repair of a torn cruciate ligament involves replacing the broken ligament by grafting a transplant (such as the hamstring tendon, patellar tendon, or quadriceps tendon). The goal of the procedure is to restore the stability of the knee to the injured person. So they can regain their physical and athletic abilities.
WHAT ARE THE ACL AND PCL?
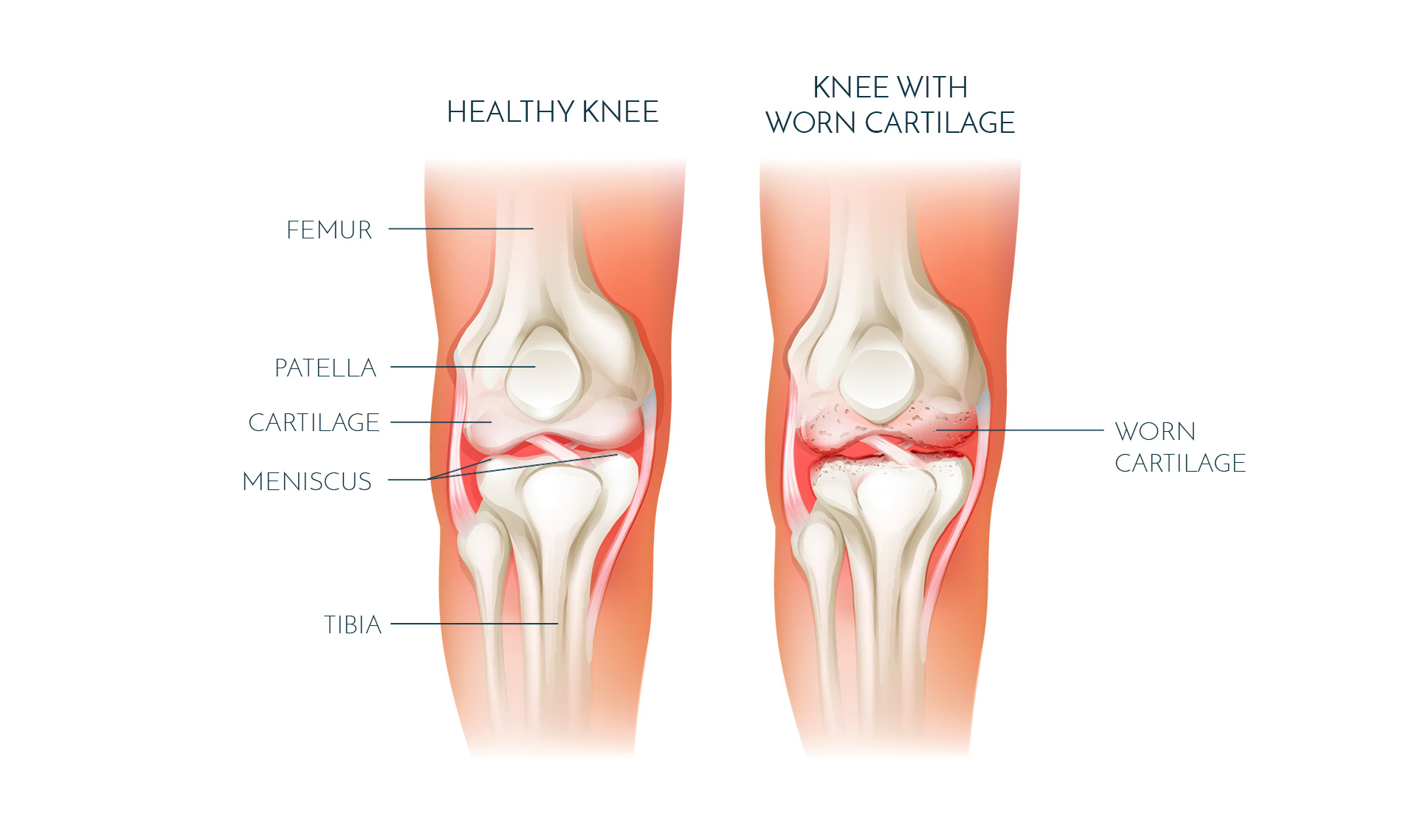
The anterior cruciate ligament (ACL) is located in the middle of the knee (part of the “central pivot”). Positioned in the notch of the femur, a true cavity in the middle of the knee, it is oblique upwards, backwards, and outwards. The posterior cruciate ligament (PCL) is located just behind it. These two ligaments are “crossed” with respect to each other: when the tibia rotates inward, they tend to wrap together. These two ligaments ensure the stability of the knee from front to back and in rotation.
IN WHAT CONTEXT WOULD ONE NEED A CRUCIATE LIGAMENT REPAIR?
The most common rupture is that of the ACL. It should be known that a rupture of the cruciate ligament does not heal naturally. Therefore, it needs to be treated, either through rehabilitation therapy or through surgery when rehabilitation and medical treatments do not work. In any case, a torn cruciate ligament must be treated because, in the long run, if not treated properly, it can lead to osteoarthritis..
Surgical Intervention and Implants
There are currently several techniques for repairing the cruciate ligament of the knee.
- The KJ Technique
The KJ (Kenneth Jones) technique involves replacing the ruptured ligament using a graft from the patellar tendon. This graft will consist of two bone sticks.
- The STG Technique
The STG (Semi-tendinous Gracilis) or ST4 (only the semi-tendinous) techniques involve harvesting the tendons of the Hamstrings to repair the ruptured cruciate ligament.
WHAT IMPLANTS ARE USED FOR ACL REPAIR ?
Interference screws :
These screws are inserted into the femoral and tibial tunnels. They wedge the graft between the tunnel wall and the graft itself. The screw can be metallic (visible on X-rays), but most of the time surgeons use absorbable screws (invisible on X-rays). Interference screws are available in various lengths and diameters to best fit each patient’s anatomy.

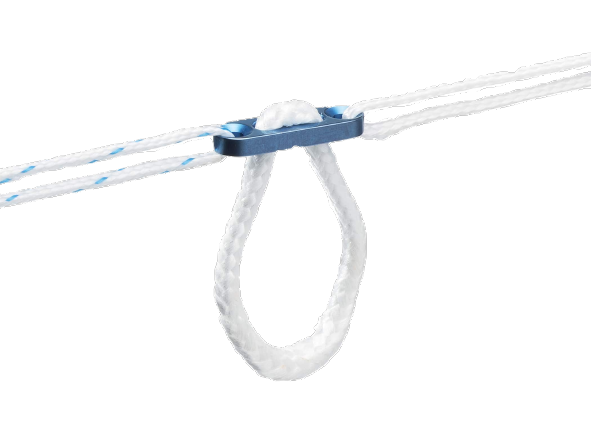
Buttons :
These are buttons mounted with a looped wire, allowing traction of the graft through the tunnel. Once the graft has migrated into the tunnel, the button flips and presses against the outer cortical bone.
Rotator cuff repair is a procedure involving the repair and reinsertion of the tendons of the rotator cuff around the head of the humerus. This procedure is most commonly performed arthroscopically. The goal of the intervention is to reintroduce the tendon around the humerus in the level of the foot print.
WHAT IS THE ROTATOR CUFF?
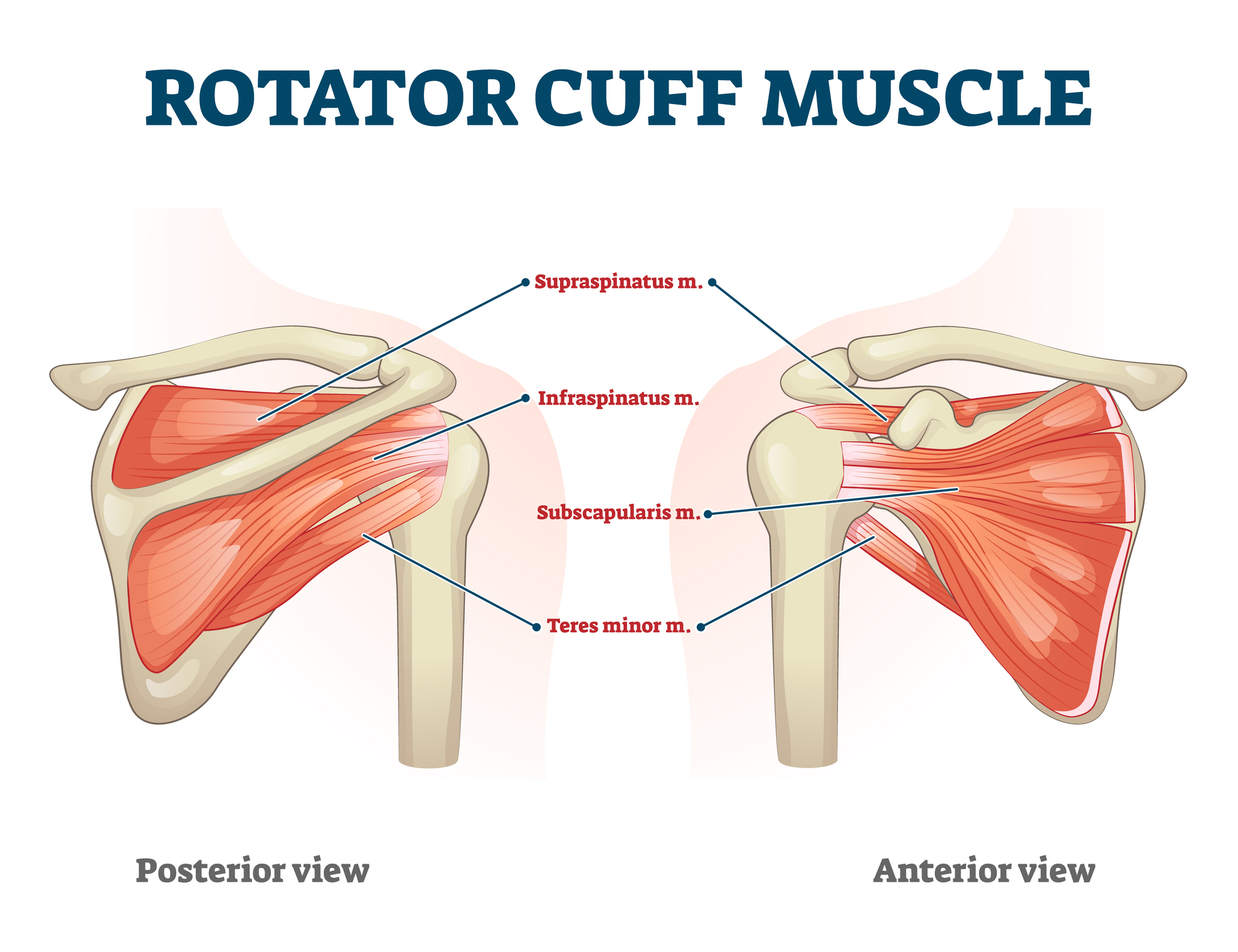
The rotator cuff is composed of tendons that connect the muscles to the bones of the shoulder. These tendons insert around the head of the humerus, and the muscles attach at various levels on the scapula. The rotator cuff thus participates in the movement of lifting the arm and its rotation.
Sometimes these tendons tear, and at that point, it is referred to as a rotator cuff tear. Most often, the tear can be degenerative, and occasionally it can be traumatic. The acromion, which is part of the scapula, forms a roof that covers the joint. Over time, the acromion may deform and form a sharp point that wears down the rotator cuff with repeated contacts. It is this repeated contact and friction that can cause the rotator cuff tear.
IN WHAT CONTEXT IS ROTATOR CUFF REPAIR NEEDED?
Rotator cuff tear can manifest as the rupture of one or several tendons (infraspinatus, supraspinatus, and subscapularis). This rupture is characterized by pain, loss of strength, and notably, a reduction in the range of motion for both rotation and lifting the arm.
If left untreated, a rotator cuff tear can lead to an increase in the widening of the tear, rendering the tendons inoperable and exacerbating the aforementioned symptoms. Additionally, the rotator cuff serves to prevent the degradation of the shoulder joint.
Surgical Procedure and Implants
Repairing the rotator cuff involves pulling the damaged tendon and reattaching it to its natural insertion point, which is around the head of the humerus.
This procedure is primarily performed arthroscopically. A camera is inserted into the shoulder, and instruments and implants suitable for this type of surgery are used to avoid opening the shoulder and carry out the repair through small incisions.
The surgical procedure unfolds in several stages:
- Cleaning of inflamed tissues.
- Acromioplasty to prevent reproducing the damage caused during the initial tear.
- Placement of anchors and sutures in the torn rotator cuff to pull and attach them to the bone.
- Depending on the extent of the rotator cuff tear, there are several repair methods such as single-row or double-row reinsertions.
WHAT IMPLANTS ARE USED FOR REPAIRING THE ROTATOR CUFF?
Shoulder anchors:
Shoulder anchors are essential elements for a proper repair of the rotator cuff. Like anchors of a boat, they are fixed into the bone and secured with wir/tape . These wires/tapes, once passed through the rotator cuff, will allow pulling the cuff towards the anchor and applying the tendons against the bone.
There are different types of anchors and materials for the rotator cuff, each presenting useful characteristics for the surgical procedure:
Types of anchors:
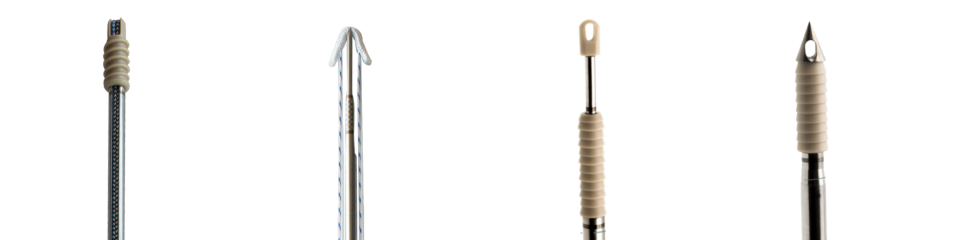
Screw anchors
Soft Tissue anchors
Impact anchors
Knotless anchors
Materials: Peek anchor, Titanium, or bioresorbable, …
Wires and tapes:
Wires and tapes are at the heart of rotator cuff repair.
They ensure proper traction of the cuff for tendon application to its natural insertion zone.
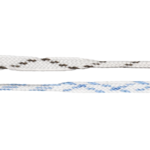
Wires must be resistant to traction and strong to ensure stable cuff repair.
Moreover, the use of tapes can be beneficial to reinforce a cuff that is more fragile than usual. tapes offer greater reinforcement by increasing their support surface on the torn cuff, thus avoiding ischemia to the tendons.
Wires and tapes are essential in any assembly of the rotator cuff, with or without knots, in single or double rows.
Dedienne Santé
A french brand’s roots
Menix Group
About
Partners
Sharing our experiences
PROFESSIONALS
PATIENT’S SECTION
COMPANY
NEWS
Made in France
